What is Psoriatic Arthritis?
Psoriasis is a skin disease in which patients have dry, red and scaly skin rashes that can occur on any part of the body. Between 5-20% of patients with psoriasis may develop an associated arthritis. Arthritis means inflamed joint. A normal joint consists of two cartilage-covered bone surfaces that glide smoothly against one another. In psoriatic arthritis, the lining of the joint – the synovium – becomes inflamed and swollen. The swollen tissues stretch supporting structures of the joints, such as ligaments and tendons. As these supporting structures stretch out, the joints become deformed and unstable. The gliding surface wears out, and joint cartilage and bone erode. In addition to the hands, psoriatic arthritis can affect joints in the spine, feet, and jaw.
How does psoriatic arthritis affect the hand?
The process of joint changes in psoriatic arthritis is very similar to the process seen in rheumatoid arthritis. The joints look red and swollen. Sometimes they feel warm. Patients have decreased motion and stiffness. While psoriatic arthritis can look very similar to rheumatoid arthritis, there are differences between the two diseases. Psoriatic arthritis tends to:
- affect men and women equally.
- affect joints asymmetrically (What occurs in one hand may not occur in the other).
- result in red, dry, scaly skin lesions rather than distinct nodules (see Figure 1).
- swelling in the middle (PIP) joints and deformities of the end (DIP) joint of the fingers first, rather than the large finger joint (MCP joint), wrist, or over tendons.
 Figure 1: Scaly, red, dry skin patches from Psoriasis on wrist
Figure 1: Scaly, red, dry skin patches from Psoriasis on wrist
Signs and symptoms of psoriatic arthritis of the hand:
Stiffness, swelling, and pain are symptoms common to all forms of arthritis, and sometimes it can be difficult to determine which type of arthritis you have. Findings classic for psoriatic arthritis include:
- diffusely swollen finger—sausage digit—especially the middle joint in the finger (PIP joint) (see Figure 2).
- pitting, ridging, or crumbly appearance of nails.
- deformity at the end joint (DIP) of the finger.
- dry, red, scaly skin patches which can occur anywhere, including the earlobe and hairline.

Figure 2: Sausage finger with swelling of the middle joint (PIP)
How is psoriatic arthritis diagnosed?
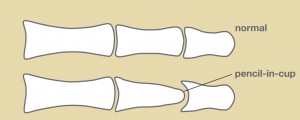
The diagnosis of psoriatic arthritis is made based on clinical examination, x-rays and lab tests. You will be asked questions about your symptoms and how the disease has affected your activities. Psoriasis and psoriatic arthritis can run in families, thus your physician will ask if family members have psoriatic arthritis or have symptoms similar to yours. A detailed examination of your hands is important because the clinical appearance helps to clarify the type of arthritis. X-rays are also helpful. Psoriatic arthritis patients often have osteolysis—loss of bone—on their x-rays. The pencil-in-cup deformity at the DIP joint is classic for psoriatic arthritis (see Figure 3). Other x-ray findings seen in psoriatic arthritis include swelling of non-bony structures, joint space narrowing, joint erosions and/or spontaneous joint fusions.These findings can occur with erosive osteoarthritis and rheumatoid arthritis as well.
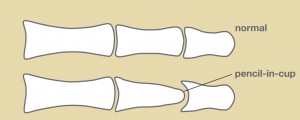
Figure 3: Pencil-In-Cup deformity of end joint of finger. Note loss of bone, narrowing/tapering of the middle bone
like a pencil, and cup shaped distortion of the end bone at the joint.
There is no lab test specifically for psoriatic arthritis. Patients thought to have psoriatic arthritis often will have labs drawn to make sure they do not have rheumatoid arthritis or gout. Patients with psoriatic arthritis will often have an elevated inflammatory marker known as the sedimentation rate (ESR) but a negative rheumatoid factor (RF). Psoriasis is part of a larger group of inflammatory arthritis called spondyloarthropathies. On occasion, other lab tests may be requested to further characterize your arthritis. Sometimes a skin biopsy may be performed in a patient with hand symptoms and a skin lesion suspicious for psoriasis, without a known history of the disease.
Treatment of Psoriatic Arthritis
Treatment for psoriatic arthritis aims to decrease inflammation, relieve pain, and maintain function. While there is no cure for psoriatic arthritis, medications are available to lessen symptoms and improve function. Optimal care involves a team approach among the patient, physicians, and therapists. The care of the psoriatic patient requires not only a hand surgeon but also a hand therapist, rheumatologist, and the patient’s primary care physician. The rheumatologist is often the physician that monitors and decides the specific type of medicine that is felt to be the most effective at that stage in the patient’s disease process.
The hand therapist will provide instruction on how to use your hands in ways to help relieve pain and protect joints. They may provide exercises, splints, wraps, and adaptive devices to help you cope with activities of daily living.
Psoriatic arthritis can be a progressive disease. Surgical interventions need to be appropriately timed in order to maximize function and lessen pain. Patients with psoriatic skin lesions are at increased risk for a surgical infection, so good control of the skin lesions is an important consideration when scheduling surgery.
There are many types of procedures to treat joints affected by psoriatic arthritis. The procedures range from joint replacements to joint fusions. The specific procedure(s) depends on many factors. These factors include the particular joint(s) involved, the degree of damage present, and the condition of surrounding joints. One of the most important factors in deciding the correct surgical procedure is the needs of the patient. There are often many ways to treat hand deformities in psoriatic arthritis. Your hand surgeon can help you decide on the most appropriate treatment for you.
What happens if you have no treatment?
Psoriatic arthritis can manifest itself with different joint findings and symptoms, and these symptoms can change over time. Consequently it has been difficult to identify an individual marker for the disease. Psoriatic skin lesions do not correlate with the severity of joint involvement. Many studies show that appropriately prescribed medication can improve function and decrease pain and swelling. Studies looking at newer agents have shown delays in X-ray changes which are felt to demonstrate a slowing of the disease process. Further work is needed to understand how and to what extent medication alters the disease process.
Download the PDF on Psoriatic Arthritis